Improving effective health coverage: are financial incentives the right remedy?

In this blog, Damien de Walque and Eeshani Kandpal from the World Bank talk to Xiaoran Xu about their latest policy research report, “Improving Effective Coverage in Health: Do Financial Incentives Work?” published in May 2022.
Healthcare coverage has increased in low- and middle-income countries (LMICs) in the last decades, yet health outcomes have remained poor. By linking remuneration to the standard of work of the health worker, performance pay seeks to improve the quality of health services by improving worker effort. However, the report finds that about two-thirds of the determinants of poor quality in primary health care in LMICs cannot be attributed to poor worker effort, meaning that performance pay is unlikely to serve as the sole remedy. Health financing reforms that focus on how and in what sequence financial incentives are implemented – while pursuing alternate policy options – can help to develop high-quality health systems and address constraints to improving effective coverage.
Performance-based financing
Since the late 2000s, more than US$2.5 billion has been invested in performance-based financing (PBF) projects in primary health service delivery in low-income countries. PBF projects held appeal for development agencies and donors because of their explicit links to transparency and accountability.
Paying for performance is a common contracting approach to deal with the principal-agent problem by tying prices to actions. It is used across public sector bureaucracies of education, infrastructure, agriculture, public-private partnerships, contracting with non-profits, and health. The goal is to improve the efficiency of public expenditure.
Financial incentives for improved health outcomes
Health PBF projects deploy a package of interventions that includes not only performance pay but also frontline autonomy, transparency/accountability, and community engagement. The idea gained prominence due to frustrations with the status quo of sustained progress in service utilisation but limited gains in health outcomes, especially among the poor. Through PBF, facilities and/or frontline workers receive payments for performance on specific predetermined indicators, as opposed to low-powered incentives like flat salaries and fixed facility budgets.
The logic is straightforward: the better a facility and its workers perform on key measures, the more financing they receive. Therefore, if poor worker effort or facility performance is the barrier to improving health outcomes, then the explicit linkage between health financing and worker and facility performance should increase the supply or quality of health services provided.
Coverage vs. effective coverage
Effective coverage is a metric that combines simple health coverage with minimum content and quality, as these are crucial to understanding why increases in service utilization may not translate into improved health outcomes. Much of the report uses effective coverage as a measure of performance.
We can look at the illustrative example below of antenatal care (ANC) amongst five sub-Saharan African countries – Cameroon, the Central African Republic, the Democratic Republic of Congo, Nigeria, and the Republic of Congo.
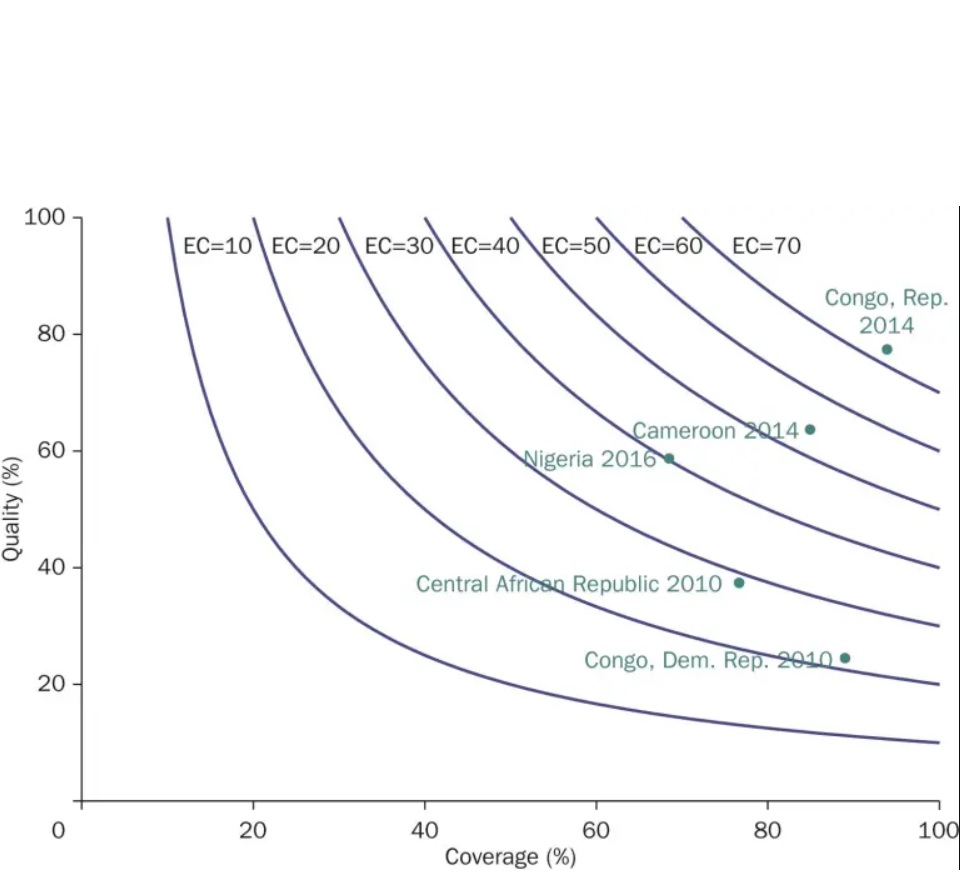
Coverage : Percent of women giving birth who had 1+ ANC visits Quality: Of these , percent who had : 4+ visits , 1+ visits with skilled provider, blood pressure taken , and blood and urine samples taken (i.e. correct treatment ). Data source: MICS
The example demonstrates a consistent – and often large – gap between coverage and effective coverage in ANC. For the best performer, the Republic of Congo, coverage is near universal, but effective coverage is below 80%. For the worst performer in terms of effective coverage, the Democratic Republic of Congo, the gap is 4.5-fold: approximately 90% of all women receive ANC, but only about 20% receive effective ANC.
Key constraints to effective coverage
We find evidence of constraints reflected by a three-gap model:
- Structural capacity gaps: Despite decades of investments in infrastructure, the availability of equipment, supplies, and drugs that are necessary for the provision of basic ANC is far from universal.
- Knowledge gaps: While some basic aspects of ANC are well known, knowledge of protocol is far from universal, with particularly low levels of knowledge of preventive care and counselling.
- Underused capacity/know-can-do gap: When health workers have all the necessary structural capacity and knowledge but still fail to perform the necessary actions.
Amongst these, we find that two-thirds of poor quality cannot be attributed to poor worker effort, meaning that performance pay is unlikely to be a silver bullet. Wealthier women are also three times as likely to receive high-quality care than poorer women, suggesting lots of within-country variation in facility quality and within-facility inequality of user fees and patient information.
Therefore, we believe the full range of constraints to quality needs to be assessed before designing interventions to improve quality.
Policy alternatives to leverage financial incentives
We compared coverage and effective coverage impacts of PBF projects to demand- and supply-side financial incentives, including conditional cash transfers (CCTs), voucher programmes, and direct facility financing (DFF). DFF sends funds directly to the front-line facilities, with more autonomy and accountability but without an explicit pay-for-performance mechanism.
The comparison shows that the mean effects are similar in size and significance across PBF projects, vouchers, and CCTs. Only for ANC visits do we observe a statistically significant difference, with CCTs and vouchers having larger effects than PBF. We also find that DFF, which includes facility-level autonomy and supervision reforms, can improve coverage and effective coverage to a similar degree as PBF, often at lower cost.
We find that there is little evidence to support across-the-board performance pay in under-resourced health systems, and performance pay is often a complex intervention which can be difficult to scale.
Optimizing performance pay outcomes
Performance pay – as one health financing approach in an arsenal of several options – should not be a “yes” or “no” question but rather a “how” and “in what sequence” question. There are a few key principles that we believe are essential for sustainable health financing reform:
- Send funds to the frontline
- Ensure transparency and accountability through good facility financial management
- Introduce routine supportive supervision if necessary
- Introduce an output or performance orientation– this can be through dashboards or portals and not just performance pay
- Unify the payment system
As countries seek to leverage health financing reform to develop high-quality health systems, we believe there is a need for an expanded suite of policy options, including but not limited to PBF, which can help countries address all the barriers they face to improving effective coverage.
Improving Effective Coverage in Health: Do Financial Incentives Work?
Improving Effective Coverage in Health: Do Financial Incentives Work? is a new World Bank Policy Research Report that builds on the rigorous body of evidence accumulated on performance-based financing (PBF) to examine the impacts of PBF and draw lessons for the future of health financing. Financial incentives and performance pay to frontline health facilities and workers have gained popularity as an innovative approach to confront the challenge of poor health outcomes in low-income countries. This approach was a significant departure from previous financing that had little link to results and accountability. PBF projects included such financial incentives as well as transparency and accountability reforms.
Damien de Walque is a Lead Economist in the Development Research Group, World Bank. His research interests include health and education and the interactions between them. He is currently evaluating the education and health outcomes of conditional cash transfers linked to school attendance and health centre visits in Burkina Faso.
Eeshani Kandpal is a Senior Economist in the Development Research Group of the World Bank. Her research examines two types of financial incentives: (1) cash transfers to poor households and (2) pay-for-performance contracts with health workers and facilities to improve the provision of primary health care. She is particularly interested in design elements like the targeting mechanisms of cash transfers and optimal pricing regimes for health service delivery as well as spillovers from incomplete contracts or targeting methods.
Xiaoran Xu is Communications and Marketing Officer at the Department of Health Policy, LSE.
This first appeared on Global Health at LSE.
Image: USAID Ethiopia via Flickr (CC BY 2.0)


