From Calamity to Equity: Global Health in the Era of Polycrisis

Cameron Boyle discusses the myriad challenges facing global health and the steps the UK Government must take to achieve health equity.
We are living in an era of polycrisis. Global crises are amplifying, accelerating and synchronising, with huge implications for human and planetary wellbeing.
One such crisis is conflict. 2022 was the deadliest year since the Rwandan genocide in 1994, while 2023 saw the highest number of conflicts since the end of World War 2. As well as the obvious effects of war on mental and physical health, healthcare itself is a frequent target. In Gaza, the rate of attacks on healthcare has been higher than any other conflict globally since 2018, averaging 73 attacks per month.
Alongside this - and in part engendered by it - soaring global temperatures have triggered a rise in natural disasters such as floods, droughts and wildfires. These weather and climate events affect health directly and indirectly, increasing the risk of death, non-communicable diseases (NCDs), the emergence and spread of infectious diseases as well as interrupting healthcare provision.
COVID-19 too, cannot be overlooked. The pandemic caused 14.6 million excess deaths and a loss of 336.8 million years of life globally in 2020 and 2021, with populations such as ethnic minorities and persons with disabilities most impacted. As health systems became overwhelmed, other diseases proliferated, creating a vicious cycle of need and suffering.
To navigate this bleak reality, one would expect wealthy nations like the UK to ramp up health spending. In fact, the opposite has happened. Between 2020 and 2021, the UK slashed Official Development Assistance (ODA) for health from $1.5bn to $763m, fuelling the fire of this dire situation.
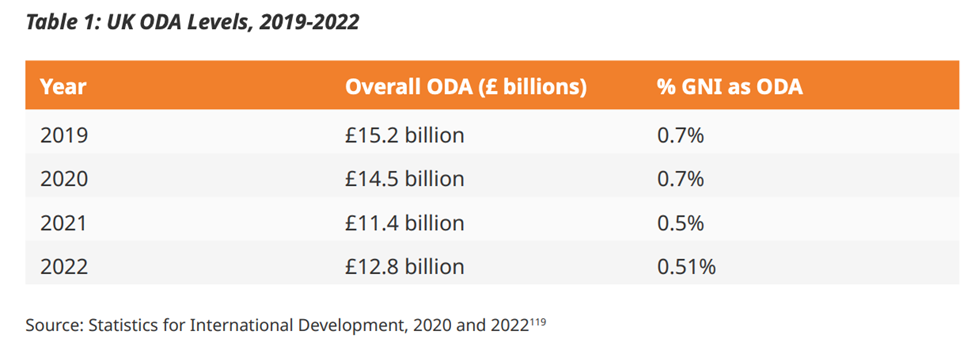
The drop in spending on health has been precipitated by a dramatic decrease in overall ODA spending (Action for Global Health / Stocktake Review)
The impact of cuts
The impact is being felt in all four corners of the globe. In Bangladesh, efforts to address NCDs have been disastrously hindered.
Concern Worldwide’s ‘Essential health for the disadvantaged’, an A+ rated programme, started in 2019 and was due to run until 2022. But in April 2021, it was given three days’ notice to cease all activities. Its target was to reach 2.6 million people, including 140,000 with disabilities, but fell short by 800,000, shedding light on the real-life impact of cuts.
Its cessation had a direct impact on health equity. Bangladesh has some of the highest out-of-pocket health expenditure in the world - much of which is spent on NCD treatment - so the project included health vouchers to reduce this expenditure.
When the cuts came, health workers informed recipients that the vouchers were now worthless. This eroded trust and was compounded by workers not knowing how to justify the decision.
In Sierra Leone, cuts meant ambulances were left without enough fuel, resulting in patients with severe health complications not being taken to hospital. 70% were women and children. 300 people went without referrals as a result, no doubt leading to fatalities.
As colliding crises take their toll, the need to reverse this damage could not be more vital. The key question is: how do we get there?
The route forward
Through its Stocktake Review, Action for Global Health provides the roadmap for progress. A fusion of achievable goals and actionable steps, it is a blueprint for achieving health equity against a backdrop of crisis.
One such step involves increasing support to national strategies that advance universal health coverage, ensuring they reach the furthest behind first. As seen in the Bangladesh example, ODA cuts have directly increased out-of-pocket expenses, widening a key barrier to health for all. Health expenses are anathema to equitable access - by supporting countries to reduce these expenses, the UK can contribute to a world where no one is left behind.
The Stocktake Review also advocates for all health programmes to make clear how they will tackle inequalities. Restoring funding is important, but not enough. The UK Government must take an intentional approach to inequity, elucidating how every action is conducive to eradication.
Dr Moira’s story
Through the Bangladesh and Sierra Leone examples, the devastating impact of ODA cuts are plain to see. But Dr Moira Chinthambi’s story shines a light on the positive difference that development spending - and more broadly, prioritising health equity - can make. Dr Moira, an ophthalmologist in Malawi, works as part of Sightsavers’ inclusive eye health programme, funded by the UK Government through UK Aid Match.
The programme aims to prevent avoidable blindness in people with and without disabilities. It enables experts like Dr Moira to go into communities and conduct outreach clinics and surgeries. As well as delivering life-changing medical care, this directly redresses inequities. In Malawi, avoidable blindness in adults often necessitates children dropping out of school, creating cycles of poverty and denying them a childhood.
By delivering accessible, equitable eye services, Sightsavers ensure that people can become more productive, go about their lives and earn a living. To quote Dr Moira: “What has been done so far has made a huge difference in the lives of so many people. I hope, in the future, we may have similar projects.”
This offers insight into what the Stocktake Review’s ambitious vision can achieve. And vision is critical - one project can make a monumental difference, but this can only be replicated at scale by a broader strategy rooted in equity.
Vision into action
Ultimately, it is now down to the UK Government to implement the steps laid out in the Stocktake Review. In doing so, it will not only take bold strides towards health for all, but show leadership on how to navigate the myriad threats to public and planetary health.
This is the view taken by Smitha Sadasivan, Senior Advisor for Inclusive Health Policy at Disability Rights India Foundation and Stocktake Review Advisory Group member:
“As the UK has taken a significant step towards the global commitment on Universal Health Coverage, such leadership in the global health space should be complemented by other member states/political leadership in a collaborative manner to ensure health equity for all population groups on this planet.”
With a new government settling into post, there is a perfect opportunity for this leadership to come to the fore. A better future will not write itself; those in power must seize the initiative and advance equity in the midst of calamity.
Cameron Boyle is Senior Digital Campaigns and Media Advisor at Action for Global Health.
Top photo: © Sightsavers/Thoko Chikondi. Dr Moira Chinthambi is seen at Kabudula Health Centre in Lilongwe Central Malawi.